Cracking Cancers Code: How Precision Medicine Is Changing the Game
Published Date: July 17, 2025
Imagine a world where your cancer treatment is as unique as your fingerprint. No more trial-and-error. No more “let’s see if this works.” Instead, a therapy plan built specifically for you—based on your genes, your lifestyle, and your tumour’s unique biology. This isn’t science fiction anymore. This is precision medicine, and it’s already transforming cancer care across the globe.
What is precision medicine, really?
At its core, precision medicine (also called personalised medicine) is all about tailoring medical treatment to the individual characteristics of each patient. In cancer care, that means using detailed information about a person’s genes, environment, and lifestyle to design the most effective treatment possible.
Traditional cancer treatment often takes a blanket approach—if two patients have lung cancer, they might both get the same chemo. But their cancers may be driven by completely different genetic mutations. Precision medicine flips this model, focusing on what’s happening at the molecular level to guide therapy.
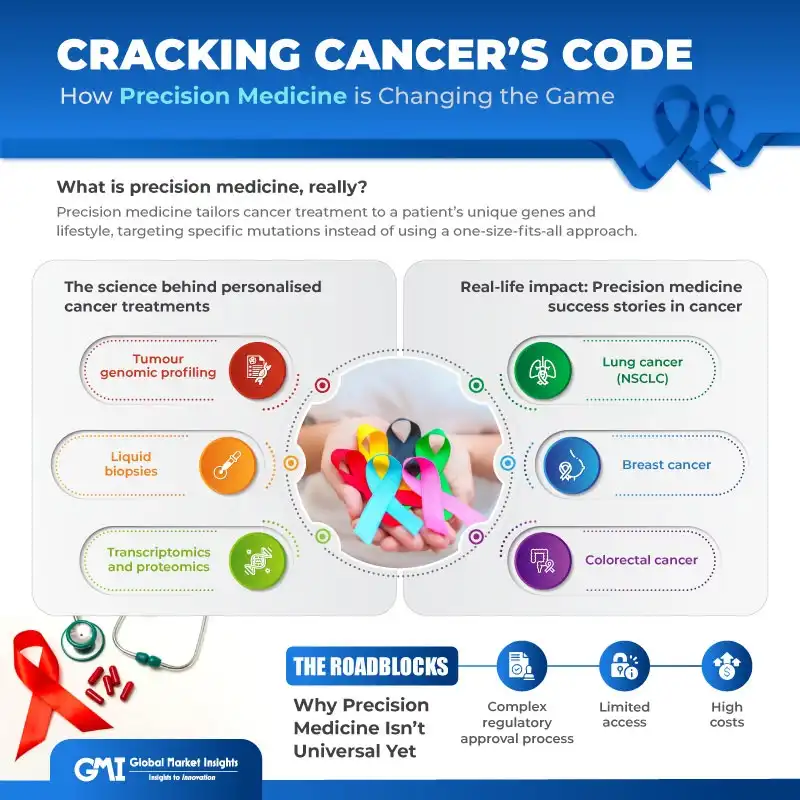
- Tumour genomic profiling: This involves sequencing the DNA of cancer cells to uncover mutations or abnormalities. For instance - An EGFR mutation in a lung tumour suggests a patient may respond well to EGFR inhibitors. A BRAF mutation in melanoma might be treated with BRAF-targeted therapy. Considering such variations in genetic mutations, in April 2023, Agilent Inc. launched the Agilent SureSelect Cancer CGP Assay designed for somatic variant profiling for a broad range of solid tumor types. The pan-cancer assay design is based on an NGS panel comprising 679 genes globally curated from leading cancer databases and in partnership with key clinical cancer researchers. The assay workflow being efficient, automatable, and flexible, made tumour molecular profiling more accessible to the broad clinical research community.
- Liquid biopsies: Instead of cutting out a tumour, doctors can now detect cancer DNA floating in the bloodstream. These non-invasive tests help monitor treatment response or spot resistance mutations without another painful biopsy.
- Transcriptomics and proteomics: Going beyond DNA, researchers also look at RNA and proteins to understand how genes are being expressed. This provides a full picture of tumour behaviour. In May 2020, SomaLogic announced its SomaSignal Proteomics for Precision Medicine Initiative. It is the first clinically focused, large-scale, partnership effort with innovators that aimed at equipping healthcare professionals with the power of proteomics technology to inform decision at the point of care.
Precision medicine offers a solution by enabling the development of therapies that specifically target the genetic mutations responsible for cancer progression. By focusing on the molecular profile of each tumor, these treatments not only enhance effectiveness but also minimize side effects, making them a preferred approach—particularly for difficult-to-treat cancers. This precision-based approach is reshaping cancer care and driving advancements in oncology.
Real-life impact: Precision medicine success stories in cancer
- Lung cancer (NSCLC): Non-small cell lung cancer used chemotherapy and low survival rates. But today, if testing reveals an EGFR, ALK, or ROS1 mutation, doctors can prescribe targeted drugs like osimertinib or alectinib that dramatically improve outcomes. And if the tumour has high PD-L1 expression? That patient may skip chemo entirely and go straight to immunotherapy.
- Breast cancer: Gone are the days of treating all breast cancer the same. Now we have subtypes like:
- HER2-positive, which can be treated with drugs like trastuzumab,
- Hormone receptor-positive, which responds to anti-estrogen therapy,
- Triple-negative, which may benefit from chemo or immunotherapy based on specific biomarkers.
- Plus, genomic tests like Oncotype DX help decide if early-stage patients even need chemo at all.
- Colorectal cancer: Testing for KRAS, NRAS, and MSI (microsatellite instability) has become routine. It helps predict who will respond to certain biologics or immunotherapies—and who won’t.
While precision medicine has the potential to transform patient care through innovative technologies and personalized treatment options, the clinical implementation of these can be complex. However, advanced detection technologies nonetheless play an integral role in identifying cancer at an early stage, monitoring disease progression, and assessing treatment efficacy.
Table 1 Advanced detection technologies and their use
|
Technology |
Use |
|
Liquid Biopsy |
A minimally invasive technique that analyses biomarkers from bodily fluids, such as blood, urine, or saliva, to detect and monitor cancers. It enables the detection of genetic mutations, circulating tumor DNA (ctDNA), and other molecular markers associated with cancer. |
|
Single-Cell Sequencing |
A powerful tool that examines individual cells to reveal the genetic and molecular differences between tumor cells and normal cells. This high resolution approach can provide detailed insights into the heterogeneity of tumors. |
|
Measurable Residual Disease Detection |
The use of biomarkers to detect MRD is imperative to monitoring the effectiveness of treatment and identifying early signs of relapse, as traditional imaging or biopsy methods can often miss the low levels of residual cancer cells. |
The role of AI and big data in personalised cancer care - Precision medicine generates massive amounts of data. That’s where artificial intelligence (AI) steps in, analysing complex patterns and helping doctors make smarter decisions.
AI in Action:
- AI tools predict how a tumour will respond to specific drugs.
- Machine learning helps match patients to clinical trials faster.
- AI-powered platforms like Watson for Oncology offer personalised treatment recommendations in seconds.
A key trend influencing this evolution is the integration of AI and machine learning (ML) into oncology precision medicine. These advanced algorithms can analyse vast amounts of genomic and clinical data, thereby identify patterns and predict treatment responses with unprecedented accuracy. Such capabilities improve diagnostic precision and treatment planning, leading to more personalized and effective cancer care. For instance, AI-driven platforms are emerging to assist oncologists in selecting the most suitable therapies based on a patient’s unique genetic profile and clinical history. Similarly, AI can help identify more in-depth data from genomics, transcriptomics, proteomics, radiomics, digital pathological images (pathomics), and other data to help support clinicians in better treating hematological cancers. In addition, AI may be used to discover new biomarkers to further assist in diagnostic, prognostic, predictive, and treatment response measures to enhance patient outcomes.
New-age clinical trials: A precision revolution - Forget the old clinical trial model where thousands of patients took the same drug. Now, precision oncology trials are smaller, smarter, and more focused.
- A basket trial refers to using the same drug or intervention to treat patients who share a common characteristic, such as a genetic alteration or a specific biomarker. Currently, basket trials are commonly used in the field of precision oncology, and they have been formulated to investigate the efficacy of molecular-targeted therapies for oncogene-defined subsets of cancers across different tumor histologies.
- An umbrella trial refers to designs where multiple therapies or interventions for patients with a certain disease are stratified into subgroups according to different characteristics that include clinical features and molecular alternations. In 2018, the Food and Drug Administration (FDA) released a guidance document describing recommendations for basket and umbrella trials, providing support for these new designs.
- A recent investigation found that the number of basket and umbrella trials has rapidly increased, suggesting a wider dissemination of these trial designs. Both basket and umbrella trials use a molecular screening protocol that either permits the enrolment of different diseases with a certain characteristic or a certain disease with different subtypes. Example: A drug that targets BRAF mutations can be tested across lung, colon, and skin cancers. Similarly, LUNG-MAP for lung cancer as an umbrella trial.
- However, both trials were designed using a fixed protocol at a specific time point. This fixed model greatly limits the efficiency of clinical trials with the rapid development of precision medicine, requiring a new clinical trial design that would be adaptable and responsive to emerging evidence.
- Hence, a new trial design called the platform trial has recently been proposed, which could be used to greatly accelerate the efficiency of clinical trials. Platform trials, also referred to as multi-arm, multi-stage design trials, are those that continuously assess several interventions against a certain disease and adapt the trial design based on the accumulated data. This design allows for the early termination of ineffective interventions and flexibility in adding new interventions during the trial.
Several governments in the Asia Pacific region are promoting precision medicine through national healthcare policies and funding initiatives, especially in clinical trials. In 2022, the Australian government announced support for USD 130 million towards an innovative multi-stakeholder public-private partnership model for sustainable precision oncology, accelerating biomarker-dependent drug development through integrating clinical trials into the standard of care. These developments enable significant potential for market expansion and strategic initiatives.
The Roadblocks: Why Precision Medicine Isn’t Universal Yet
While the benefits are clear, there are still barriers keeping personalised cancer care from becoming the norm everywhere.
- High costs: While precision medicine provides highly personalized and effective cancer treatments, its high cost presents a significant barrier to widespread adoption, affecting healthcare systems, patients, and insurers. Precision oncology therapies, such as monoclonal antibodies and small-molecule inhibitors, are often priced beyond the reach of many patients. For example, Keytruda (pembrolizumab), a monoclonal antibody used to treat various cancers, costs approximately USD 11,564 for each three-week dose. Similarly, Tagrisso (osimertinib), a small-molecule inhibitor for non-small cell lung cancer, is priced at around USD 12,750 for a month’s supply. These high prices reflect the extensive research, development, clinical trials, and regulatory approvals required to bring these therapies to market.
- Limited access: Many people, especially in rural or low-income areas, can’t access advanced diagnostics or experimental treatments.
- Complex regulatory approval process: The complex regulatory approval process poses a significant challenge to the growth of the oncology precision medicine market. Precision therapies, including monoclonal antibodies and small-molecule inhibitors, must undergo a rigorous and multi-step regulatory process that involves extensive clinical trials, the co-development of companion diagnostics, and stringent assessments of safety and efficacy. Regulatory agencies like the FDA and EMA require detailed data on the genetic and molecular profiles of patients, which often demands advanced, expensive testing methods. These stringent requirements can significantly extend the time to market, driving up costs for pharmaceutical companies.
What’s Next? The Future of Precision Cancer Care –
We’re just scratching the surface. The next few years will bring incredible advances.
The future of oncology precision medicine is set for remarkable growth and transformation, driven by advancements in technology, the increasing prevalence of cancer, and a concerted shift towards personalized healthcare. This field, which focuses on customizing cancer treatment based on the genetic, molecular, and environmental characteristics of individual patients, is expected to revolutionize cancer care by enhancing treatment efficacy and minimizing side effects.
Another noteworthy advancement is the development of circulating tumor DNA (ctDNA) analysis. This innovative technique involves detecting and analysing fragments of DNA shed by cancer cells into the bloodstream, providing a non-invasive method to monitor tumor dynamics, detect minimal residual disease, and identify emerging resistance mutations. ctDNA analysis is invaluable for tracking treatment effectiveness in real-time and enabling timely adjustments to therapy plans. For example, Guardant Health’s Guardant360 test is a leading ctDNA-based liquid biopsy that offers comprehensive genomic profiling from a simple blood draw, facilitating personalized treatment decisions. Similarly, drugs like larotrectinib, approved for any tumour with an NTRK fusion regardless of type, signal a shift toward biology-based approvals, not location-based ones.
Moreover, functional precision medicine is gaining traction as a complementary approach to genomics-guided therapy. This method involves testing a diverse range of drugs on a patient’s cancer cells cultured outside the body to determine the most effective treatment. By directly assessing drug sensitivity, functional precision medicine can provide actionable insights even when genomic data is inconclusive. For instance, researchers at the Medical University of Vienna have successfully employed this approach to identify effective treatments for patients with treatment-resistant blood cancers.
In addition to technological advancements, strategic collaborations and partnerships are essential for the growth of the precision oncology market. Pharmaceutical companies are joining forces with diagnostic firms and research institutions to develop and commercialize innovative precision therapies. For example, ConcertAI and LabCorp have partnered to enhance precision oncology research by launching clinical studies aimed at improving patient retention and ensuring equitable access to research as a care option.
Why Precision Medicine Is Here to Stay
Cancer is no longer a one-size-fits-all disease, and we can finally stop treating it that way. With the rise of precision medicine, we are entering a new era—one where treatments are smarter, side effects are lower, and outcomes are better.
Sure, there are challenges to overcome. But the progress we’ve made is nothing short of remarkable. From lung and breast cancer to melanoma and beyond, personalised treatments are giving patients real hope. As technology continues to evolve, and access improves, we can expect precision medicine to become the standard of care, not the exception.





