The Medical Bill Shock Syndrome – And How to Cure It
Published Date: September 10, 2025
Healthcare costs remain one of the most pressing challenges for healthcare providers, patients, and policymakers worldwide. Growing expenditures, opaque billing systems, and limited access to cost information have left patients unsure about what they will ultimately pay for services until after care is delivered. In response, healthcare price transparency has emerged as a transformative approach that empowers patients, builds trust in providers, and fosters competition across the industry.
In recent decades, healthcare has undergone notable transformation. Technological advancements in diagnostic capabilities, treatment protocols, and medical technologies, have significantly improved prevention, early detection, and disease management. Yet these very innovations have also driven unprecedented increases in healthcare spending. For policymakers, healthcare providers, and healthcare payers, the challenge is no longer simply to separate effective interventions from ineffective ones, but to determine which services deliver the greatest value relative to their cost. For patients, the situation is even more complex: navigating a system where the true cost of care often remains hidden until long after treatment.
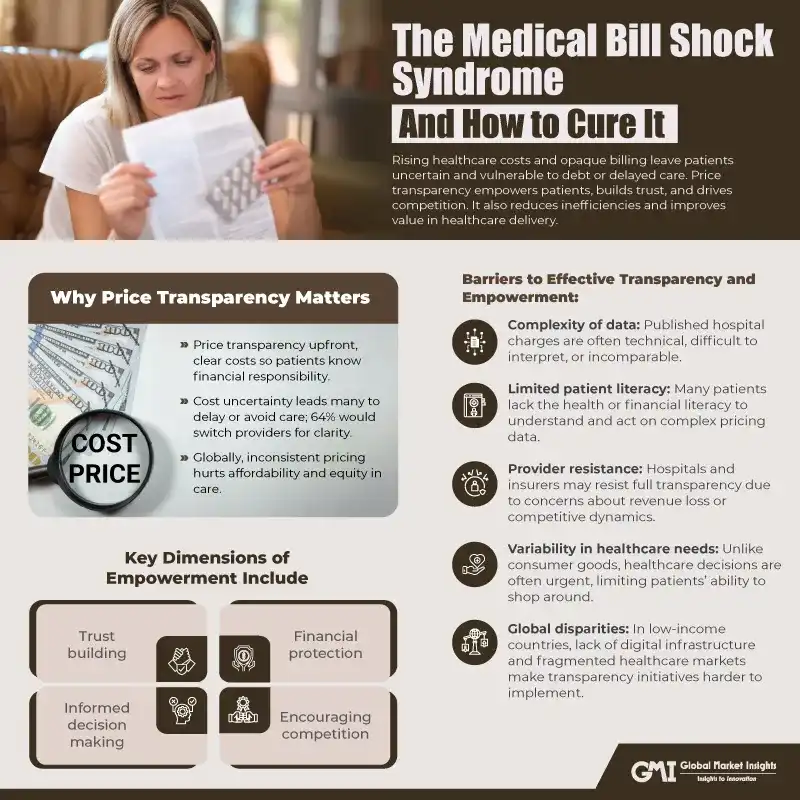
This disconnect between rising costs, opaque pricing structures, and patient expectations has made price transparency and patient empowerment urgent imperatives in modern healthcare policy and practice.
Beyond individual billing concerns, the lack of transparency contributes to the broader true cost of healthcare such as rising medical debt, surprise bills, and delayed treatments. When patients cannot anticipate expenses, many postpone necessary care or face unexpected financial strain, which in turn impacts long-term health outcomes. By addressing these hidden costs through greater transparency, providers not only empower patients but also help reduce systemic inefficiencies and financial barriers to care.
The Rising Global Cost of Healthcare
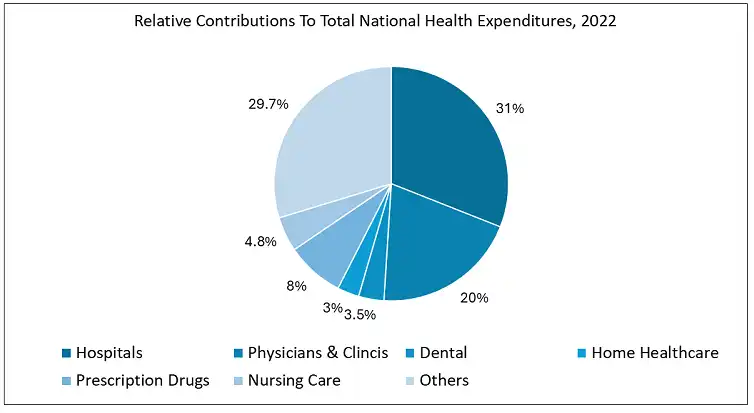
Healthcare expenditure has been increasing steadily across high, middle, and low-income countries. According to the World Health Organization (WHO), global health spending has more than doubled in the past two decades, reaching nearly 10% of global GDP by 2020. In the U.S., healthcare spending accounts for nearly 18% of GDP, the highest among developed nations. European countries such as Germany, France, and the UK spend between 9 – 12% of GDP, while emerging economies like India and Brazil spend less than 5%, often resulting in significant out-of-pocket costs for patients.
Drivers of cost escalation include:
- Medical innovation and technology: New diagnostic and treatment tools often carry high development and delivery costs.
- Chronic disease burden: Longer life expectancy has led to higher prevalence of conditions such as diabetes, cancer, and cardiovascular disease.
- Administrative complexity: Particularly in the U.S., fragmented insurance systems contribute significantly to overhead costs.
- Pharmaceutical pricing: Variability in drug pricing and patent protection increases disparities across countries.
While high income countries struggle with budget sustainability, low and middle-income countries face the dual challenge of limited resources and lack of transparency, pushing patients into financial distress.
Understanding the True Cost of Healthcare
The phrase true cost of healthcare reflects the difference between what is charged, what is negotiated, and what is ultimately paid. Patients often encounter multiple layers of pricing:
- Chargemaster rates: The list price set by hospitals, often much higher than actual payments.
- Negotiated rates: Prices agreed between providers and insurers, usually undisclosed to patients.
- Out-of-pocket payments: Deductibles, co-payments, and uncovered services borne directly by patients.
- Hidden costs: Facility fees, out-of-network charges, or follow-up procedures.
As per the Patient Rights Advocate study highlights, price variations of more than 10 times for the same care across health plans and 33 times across hospitals is observed, a disparity invisible until after care is delivered. Similarly, the Commonwealth Fund notes that surprise medical billing remains a leading cause of medical debt in the U.S., while in countries without universal coverage, catastrophic out-of-pocket costs push millions into poverty annually.
Thus, understanding the true cost is not only about the price of procedures but also about transparency in how these costs are structured and communicated.
Why Price Transparency Matters:
At its core, price transparency means giving patients access to clear, upfront information about the cost of medical services and procedures. This is not just about posting price lists, it is about enabling patients to understand their financial responsibility before undergoing treatment.
In the U.S., surveys show that nearly 6 in 10 consumers delay or avoid medical care due to uncertainty over costs. Moreover, 64% of patients say they would switch providers for greater price transparency, highlighting how central this issue has become to patient choice. Globally, similar concerns exist in both developed and emerging healthcare systems, where the lack of standardized pricing undermines affordability and equity in care delivery.
The U.S. Push for Transparency:
The U.S. has taken legislative steps to improve transparency. The Hospital Price Transparency Rule, in 2021, requires hospitals to provide machine-readable files of standard charges and consumer-friendly shoppable services. Similarly, the Transparency in Coverage Rule, in 2022, compels insurers to publish online cost-sharing estimates. While compliance has been uneven, these policies reflect a growing recognition of the need for reform.
According to the Experian, when patients receive cost estimates upfront, their likelihood of paying bills on time increases by 50%. This not only benefits providers but also reduces administrative friction in the revenue cycle. Hospitals that have adopted transparent billing practices report higher patient satisfaction and improved collection rates, underscoring the financial and relational benefits of openness.
Technology as a Catalyst:
Digital tools are playing a pivotal role in advancing transparency. Patient engagement platforms, mobile apps, and AI-driven cost estimators allow individuals to compare treatment options and anticipate out-of-pocket costs. In fact, 74% of healthcare organizations in the U.S. now consider price transparency technology a strategic priority. Globally, similar digital solutions are being deployed in regions such as Europe and Asia, where governments are also prioritizing affordability and equitable access.
Global Perspective on Price Transparency:
While the U.S. has led much of the regulatory discussion, other countries are adopting similar models. For example:
- European Union (EU) initiatives emphasize digital health records integrated with pricing to help cross-border patients make informed choices.
- In India, where out-of-pocket expenditure accounts for over 48% of total health spending, transparency is becoming essential to reduce financial distress.
- OECD countries are increasingly benchmarking healthcare costs across borders to ensure standardization and efficiency.
- These examples underscore that transparency is not just a U.S. issue, it is a global imperative for sustainable healthcare.
Patient Empowerment Through Transparency:
Price transparency, when effectively implemented, translates into patient empowerment. Empowered patients are those who have access to clear, actionable information about the cost and quality of healthcare, enabling them to make informed choices.
Key dimensions of empowerment include:
- Informed decision-making: Patients can evaluate cost alongside quality, accessibility, and personal preference.
- Encouraging competition: Providers may lower prices or improve quality to remain competitive when costs are publicly visible.
- Financial protection: By anticipating expenses, patients can avoid unexpected bills and reduce the risk of medical debt.
- Trust building: Transparency fosters greater confidence in providers and payers, reinforcing the patient-provider relationship.
For instance, according to a research study report, it was found that patients who had access to upfront cost estimators were more likely to select lower-cost facilities without compromising on quality. Similarly, Health Catalyst notes that empowering patients with transparent pricing supports preventive care, as individuals are less likely to avoid routine check-ups due to fear of hidden costs.
Globally, patient empowerment through transparency can address inequities in access. In India, for example, government initiatives like Ayushman Bharat are moving toward standardized pricing of procedures to make healthcare more predictable and affordable for low-income populations.
Barriers to Effective Transparency and Empowerment:
Despite its promise, several challenges hinder the realization of true price transparency:
- Complexity of data: Published hospital charges are often technical, difficult to interpret, or incomparable.
- Limited patient literacy: Many patients lack the health or financial literacy to understand and act on complex pricing data.
- Provider resistance: Hospitals and insurers may resist full transparency due to concerns about revenue loss or competitive dynamics.
- Variability in healthcare needs: Unlike consumer goods, healthcare decisions are often urgent, limiting patients’ ability to shop around.
- Global disparities: In low-income countries, lack of digital infrastructure and fragmented healthcare markets make transparency initiatives harder to implement.
The Commonwealth Fund emphasizes that transparency must go beyond compliance; it must focus on usability and clarity if it is to truly empower patients.
Toward a Transparent, Patient-Centred Future:
The path forward requires alignment of policy, technology, and culture.
- Technology-driven solutions: Digital tools, apps, and AI-based estimators can simplify complex pricing data into patient-friendly formats.
- Policy reinforcement: Stronger enforcement of transparency regulations, as well as expansion of coverage schemes, are needed both in the U.S. and globally.
- Education and literacy: Patient education initiatives can help individuals interpret pricing data and make informed choices.
- Global best practices:
- The U.S. leads in regulatory experimentation.
- The UK and EU demonstrate how national systems can build inherent transparency by reducing patient exposure to unpredictable costs.
- Emerging economies illustrate the importance of price caps and standardized packages for essential services.
- The U.S. leads in regulatory experimentation.
A transparent system balances cost, quality, and accessibility, making patients partners rather than passive recipients of care.
Conclusion:
The movement toward healthcare price transparency represents a fundamental shift in how care is delivered and consumed. According to the Experian’s findings, transparency is not just a regulatory obligation it is a strategic enabler of trust, payment efficiency, and patient loyalty. Both in the U.S. and globally, transparency is key to addressing the affordability crisis and creating a more equitable healthcare landscape. Ultimately, patients deserve to know the true cost of their care. By embracing transparency, healthcare systems can empower individuals, strengthen financial sustainability, and move closer to a future where healthcare is not only accessible but also predictable and fair.





