The Medication Thats Rewriting Weight-Loss Rules
Published Date: September 2, 2025
Introduction - From blood sugar control to body weight transformation
Until very recently, medical therapy for obesity delivered only modest wins. Lifestyle programs such as diet, exercise, and behaviour change, remain foundational, and bariatric surgery has been the most reliable way to produce large, durable weight loss. But over the last few years a class of medicines originally developed to treat type 2 diabetes has shown dramatic effects on body weight. The glucagon-like peptide-1 receptor agonists (GLP-1 RAs), and now next-generation multi-agonists that include GLP-1 activity, are producing average weight reductions far larger than previously expected from drugs, reshaping clinical practice and how clinicians and patients think about obesity treatment.
Obesity has long been recognized as one of the most pressing public health challenges of the 21st century. The WHO estimates that more than 1 billion people worldwide are living with obesity, a condition that significantly increases the risk of cardiovascular disease, type 2 diabetes, cancer, and premature mortality. Despite decades of lifestyle-based interventions, long-term weight loss has proven elusive for many, driving an urgent need for safe and effective medical therapies.
Glucagon-like peptide-1 receptor agonists (GLP-1 RAs), originally designed for type 2 diabetes management — have emerged as one of the most powerful pharmacological tools for sustainable weight reduction. While their glucose-lowering effects have been well documented for years, recent clinical breakthroughs have shown that these medications can deliver transformative weight loss, often rivalling or even surpassing results from bariatric surgery for certain patients.
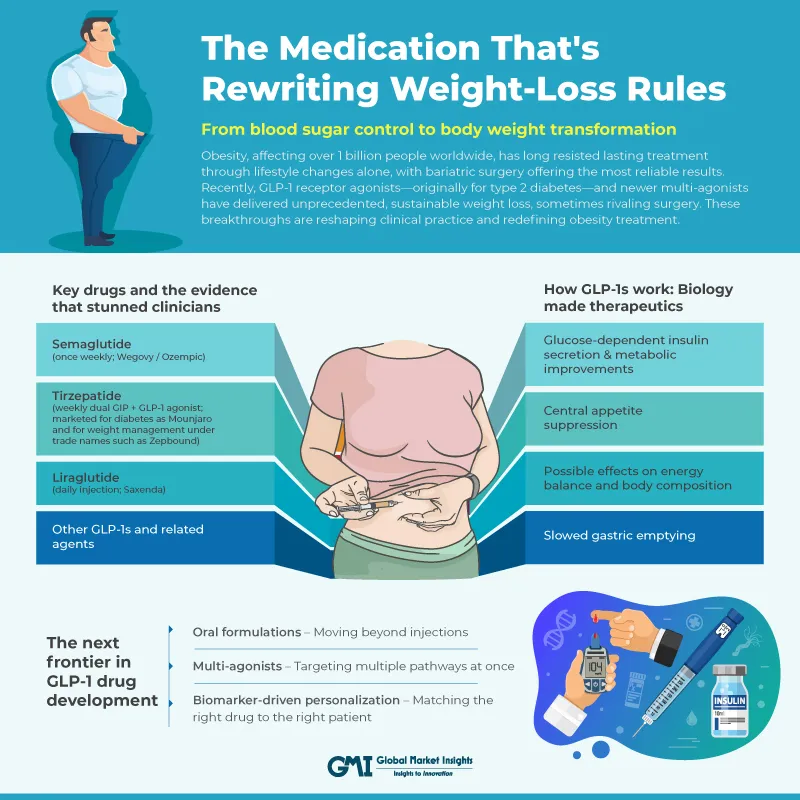
How GLP-1s work: Biology made therapeutics
GLP-1 is an intestinal hormone released after meals. It is part of the incretin system that helps the body coordinate insulin release with nutrient intake. Endogenous GLP-1 has short-lived effects, but pharmaceutical GLP-1 RAs are engineered to have far longer half-lives and therefore sustained physiological impact. Several mechanisms explain why GLP-1 RAs reduce body weight:
- Central appetite suppression: GLP-1 receptors in the hypothalamus and brainstem alter hunger signalling and food reward. Patients report decreased appetite and fewer cravings for energy-dense foods.
- Slowed gastric emptying: By delaying stomach emptying, GLP-1 RAs increase feelings of fullness and reduce meal size.
- Glucose-dependent insulin secretion & metabolic improvements: GLP-1 improves post-meal insulin secretion and lowers glucagon, which improves glycemia and can reduce metabolic drivers of weight gain.
- Possible effects on energy balance and body composition: Some data suggest modest improvements in energy expenditure and preferential loss of fat mass versus lean mass, but appetite suppression is the dominant driver of weight loss.
By combining peripheral effects (slower gastric emptying, metabolic adjustments) with central nervous system actions (reduced hunger and altered food reward), GLP-1 RAs produce sustained reductions in caloric intake and clinically meaningful weight loss.
Key drugs and the evidence that stunned clinicians
Several GLP-1 RAs and related agents have been studied for weight management. Below are the most clinically important agents and what the data show.
-
Semaglutide (once weekly; Wegovy / Ozempic)
Semaglutide is a potent, long-acting GLP-1 RA available as a weekly injectable. In adults with overweight or obesity (without diabetes) the semaglutide 2.4 mg dose produced an average weight reduction of about 15% of baseline body weight over ~68 weeks in the STEP 1 trial, a result that surprised many clinicians because it brought pharmacologic outcomes into a range previously associated with surgical interventions. The STEP program (including STEP 1 and related trials) demonstrated clinically meaningful weight loss across populations and established semaglutide as a new standard for many patients with obesity.
-
Tirzepatide (weekly dual GIP + GLP-1 agonist; marketed for diabetes as Mounjaro and for weight management under trade names such as Zepbound)
Tirzepatide combines GLP-1 and GIP receptor agonism and has shown the largest average weight losses of any medication to date. In the SURMOUNT-1 trial, tirzepatide produced dose-dependent weight reductions, with average losses approaching or exceeding ~20% at higher doses in adults with obesity who did not have diabetes, numbers that markedly exceed historical pharmacotherapy benchmarks. These results established tirzepatide as the most potent agent in the current pharmacologic armamentarium for obesity.
-
Liraglutide (daily injection; Saxenda)
Liraglutide preceded semaglutide as an approved GLP-1 option for weight management. At the 3.0 mg daily dose, liraglutide produced average weight losses on the order of ~8% in pivotal trials (SCALE program), with additional benefits in glycemic measures and cardiometabolic risk markers. While effective, liraglutide’s average weight loss is smaller than semaglutide’s and tirzepatide’s.
-
Other GLP-1s and related agents
Dulaglutide, exenatide and other GLP-1 RAs used primarily for diabetes generally produce modest weight loss compared with the agents above; their primary indication remains glycemic control. The field is rapidly moving beyond single-target GLP-1 agonism: dual and triple agonists, combining GLP-1 with receptors for GIP and/or glucagon, are designed to produce larger weight loss and beneficial metabolic effects.
Putting the trial numbers into perspective
Historically, anti-obesity drugs produced average weight losses in the single digits (5–10%), and even the best options rarely approached double-digit percentages at the population level. The semaglutide and tirzepatide trials changed that expectation:
- Semaglutide 2.4 mg once weekly produced average weight loss around 15% at ~68 weeks in adults without diabetes, with a substantial fraction of participants losing ≥15–20% of baseline weight.
- Tirzepatide (highest doses in SURMOUNT-1) produced average losses near or above 20%, depending on dose, with clear dose-response effects in pivotal trials.
- Liraglutide at 3.0 mg produced mean reductions near 8% in major trials, clinically meaningful but smaller than the newer agents’ effects.
These differences matter clinically: larger average weight loss translates into bigger improvements in blood pressure, glycemic measures, sleep apnea metrics, mobility, and quality of life for many patients. The magnitude of weight loss with semaglutide and tirzepatide places pharmacotherapy into a category that previously would have only been associated with surgical intervention.
Safety profile: What clinicians and patients must know
High efficacy always requires careful safety evaluation. GLP-1–based therapies share several common adverse effects and carry some rare but important risks. The most frequent adverse effects are gastrointestinal and dose-related:
- Nausea, vomiting, diarrhoea, constipation, and abdominal discomfort - Typically worst during dose escalation and often resolve or attenuate with continued treatment and slower titration. These effects are the leading reason patients stop therapy in real-world settings and are a predictable part of initiation.
- Less common but serious concerns - Acute pancreatitis has been reported with GLP-1 RAs. Although causality is debated and absolute risk is low, clinicians should be alert to severe abdominal pain and elevated pancreatic enzymes and stop therapy if pancreatitis is suspected.
- Gallbladder disease - Rapid weight loss, whether surgical or pharmacologic, raises gallstone risk; cholelithiasis and cholecystitis have been observed. Monitor for biliary colic symptoms.
- Acute kidney injury (AKI) - Severe vomiting or diarrhoea can cause dehydration and secondary kidney injury; advise patients to maintain hydration and seek care for persistent GI losses.
- Thyroid C-cell tumors (rodent signal) - GLP-1 RAs carry a boxed warning regarding an increased risk of thyroid C-cell tumors in rodents; although human relevance remains uncertain, patients with a personal or family history of medullary thyroid carcinoma (MTC) or multiple endocrine neoplasia type 2 (MEN2) are generally advised not to use GLP-1 RAs.
The next frontier in GLP-1 drug development
GLP-1 medications have already reshaped obesity management, but research pipelines suggest that what we have today is just the beginning. Several promising innovations are on the horizon, aimed at improving patient convenience, enhancing efficacy, reducing side effects, and tailoring therapy to individual needs.
-
Oral formulations – Moving beyond injections
Historically, GLP-1 drugs have been injectable because peptides are broken down in the digestive tract before they can be absorbed. Advances in formulation science are changing that. For example, Rybelsus (semaglutide tablets), the first oral GLP-1 approved for type 2 diabetes, has demonstrated meaningful weight loss in clinical studies, although it currently requires strict administration guidelines (empty stomach, limited fluid intake before and after dosing). Researchers are exploring nanoparticle carriers, enzyme inhibitors, and absorption enhancers to make daily oral GLP-1s easier to take and potentially more effective. Future iterations may be weekly oral tablets instead of daily dosing.
-
Multi-agonists – Targeting multiple pathways at once
While GLP-1 receptors slow gastric emptying and increase satiety, other gut hormones like GIP (glucose-dependent insulinotropic polypeptide) and glucagon also influence energy balance. Drug designers are creating multi-agonists that stimulate more than one receptor, potentially amplifying results. Example in development - Triple agonists targeting GLP-1, GIP, and glucagon are in early trials. Glucagon activation may increase calorie burning (thermogenesis) while still maintaining satiety. This combination could be particularly effective for people with stubborn visceral fat.
-
Biomarker-driven personalization – Matching the right drug to the right patient
One of the most exciting developments is the use of biomarkers, measurable biological indicators, to predict how a patient will respond to therapy. This could make obesity treatment as personalized as cancer care. Researchers are investigating genetic variants in GLP-1 receptor pathways, gut microbiome profiles, and baseline hormone levels to determine who will respond best to GLP-1 therapy, who might benefit from dual agonists, and who is more prone to side effects. Potential benefit - A patient whose biomarkers suggest rapid metabolism of GLP-1 drugs might be offered a longer-acting formulation, while someone with strong GIP responsiveness could start on a dual-agonist right away, avoiding months of trial-and-error.
List of few ongoing clinical trials involving obesity therapies
|
Drug/ Target |
Company |
Phase |
Predicted launch data |
|
Semaglutide (Wegovy) GLP1R |
Novo Nordisk |
Phase III |
Q4 2025 |
|
Cagrilintide + Semaglutide (cagrisema) CALCR; GLP1R |
Novo Nordisk |
Phase III |
Q1 2026 |
|
Tirzepatide (zepbound) GLP1R; GIPR |
Lilly |
Phase III |
Q2 2026 |
|
Orforglipron (ly3502970) GLP1R |
Lilly |
Phase III |
Q3 2026 |
|
Maridebart Cafraglutide (Maritide) GLP1R; GIPR |
Amgen |
Phase II |
Q4 2030 |
|
Efpeglenatide GLP1R |
Sanofi and HanmiPharm |
Phase III |
NA |
In short, the future of GLP-1 therapy is moving toward greater convenience, higher efficacy, and more individualized care. These innovations will not only make treatment easier for millions of people but also expand the scope of obesity management to a truly precision-medicine approach.
Conclusion
The GLP-1 revolution is one of those rare moments in medicine when a class of drugs reshapes clinical expectations. What began as diabetes therapy has matured into a powerful set of tools for obesity management, with semaglutide and tirzepatide delivering efficacy that approaches surgical outcomes for many patients. These medicines work by harnessing gut-brain hormonal pathways to reduce appetite and change food intake behaviour, a far more targeted approach than telling patients only to “eat less and move more”.
Safety vigilance, thoughtful patient selection, and integration with behavioural care are the practical requirements for translating trial efficacy into real-world benefit. At the same time, the drug development horizon is full of promising directions: oral formulations, multi-agonists, longer-acting molecules, and the emergence of biomarkers to personalize therapy.
For clinicians, GLP-1–based therapy has joined the toolkit for obesity in a way that demands attention and responsible use. For people living with obesity, these medicines offer new, scientifically grounded hope for substantial and meaningful weight loss. The revolution is underway, and with careful stewardship and continued research, GLP-1–based strategies are poised to become an integral part of comprehensive, modern obesity care.





