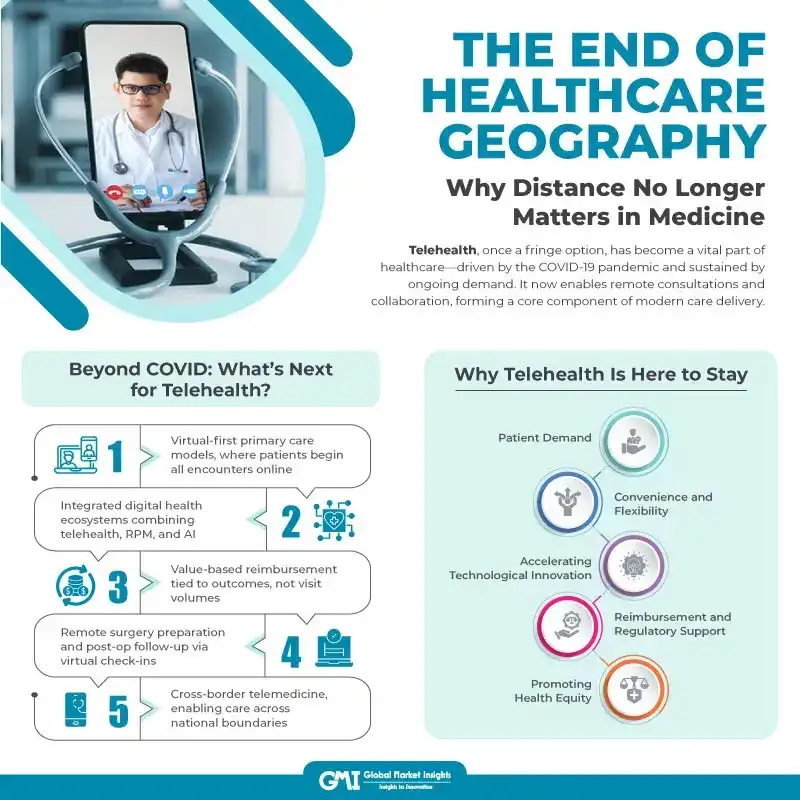
The End of Healthcare Geography: Why Distance No Longer Matters in Medicine
Published Date: August 20, 2025
Telehealth is defined broadly as the delivery of healthcare services using digital technologies that has transformed from a fringe option into a mainstream component of the healthcare system. Whether it is a video consultation between a clinician and patient or remote collaboration between providers, telehealth represents a fundamental shift in how care is accessed and delivered. While the COVID-19 pandemic catalyzed this shift, the momentum has not faded. What began as a necessary pivot in response to crisis has evolved into a durable care model. In just a few years, telehealth has gone from a convenient add-on to a critical piece of healthcare infrastructure.
The Pandemic as a Catalyst
When COVID-19 struck, patients and providers were left with few safe options for routine medical care. As a result, 41% of U.S. adults postponed or avoided in-person visits during the early months of the pandemic. Telehealth offered a lifeline, an immediate scalable solution that allowed care to continue with minimal risk of virus transmission. Hospitals restricted face-to-face appointments, and providers pivoted to virtual visits at unprecedented speed.
For many patients, particularly those managing chronic conditions or mental health concerns, virtual care became the new norm, and they adapted quickly and enthusiastically. Commercial interest in telehealth has boomed, with both start-ups and established companies, such as Amazon, providing virtual care services. An area of particular activity has been behavioral and mental health, where multiple companies are vying to provide remote counseling. For instance, the city of Reno, Nevada, instituted a USD 1.3 million experimental program in which the city paid for virtual therapy of residents through the smartphone app Talk space.
Five Years Later: A Permanent Shift
Although telehealth before and after COVID doesn’t look quite the same, that does not mean it has not continued growing. Virtual care has been thoroughly evaluated and has proven that telehealth is here to stay. The past several years have highlighted the benefits of virtual health, including increased access to care, reduced costs, and improved patient outcomes.
Five years since the pandemic's onset, the healthcare landscape has irrevocably changed. Video visits, once a novelty, are now a routine part of medical care. Surveys indicate that one in four patient visits is expected to happen within the next five years. Health systems and clinicians are rethinking care delivery with digital front doors, virtual-first care models, and remote monitoring. No where is this shift more evident than in mental health services. According to FAIR Health, telemental health visits rose from 58.8% in August to 61.2% in September 2022, reflecting growing trust in remote behavioral care. For patients in rural communities or those struggling with stigma, virtual therapy has improved both access and acceptance.
Will Virtual Care Continue to Grow?
Virtual healthcare technology is here to stay and is likely to continue to grow in popularity and importance as healthcare providers and patients embrace its benefits. The growth of virtual-first care has changed the healthcare industry for the better. Virtual-first healthcare has the potential to improve health outcomes by enabling patients to track their health data and receive personalized care plans more easily. It can also help to reduce healthcare costs by reducing the need for in-person appointments and hospitalizations. Healthcare providers and insurers are likely to continue expanding their telemedicine offerings as they see the benefits of virtual-first care in terms of improved patient outcomes, increased efficiency, and reduced costs.
In addition to improving access to care, telehealth has spurred the use of wearable and digital technologies that enable virtual care. Remote monitoring tools, including mobility trackers, blood pressure monitors and glucometers, allow doctors to monitor the health of their patients and their response to treatment. Patients engage with smartphone health apps that can keep track of other aspects of daily living that affect their health, such as nutrition data, heart rate, sleep patterns and other such parameters. The detailed and long-term monitoring that these tools provide can identify early signs of disease and has the potential to improve preventative care, as well as providing more personalized care. In realizing the ambitions of telehealth, a host of challenges will need to be faced. At this early stage in the development of this field, it remains unclear which conditions and treatments telehealth and mobile apps are effective for. Clinical studies are needed to figure out what works and what does not. Given the growing use of telehealth for mental and behavioral healthcare, the efficacy of telehealth in these settings needs to be rigorously assessed.
The Telehealth Ecosystem is Expanding
Beyond video consultations, telehealth is expanding into a broader ecosystem that includes:
- Remote patient monitoring (RPM) through wearables and IoT devices
- At-home diagnostics like lab testing kits
- Mobile health apps for medication adherence and chronic disease management
- AI-driven chatbots for triage and routine follow-ups
Companies like 23andMe and Everlywell have made genetic and diagnostic testing accessible from home, and at-home COVID tests normalized the idea of self-collected samples. Going forward, we may see mobile phlebotomy and in-home imaging services bringing healthcare to the doorstep rather than forcing patients to travel. This decentralized model turns healthcare delivery on its head: The system comes to the patient, not the other way around.
Why Telehealth Is Here to Stay
Several interlinked factors support telehealth’s long-term growth:
- Patient Demand
Today’s patients are tech-savvy and expect convenience. A study published by the American Journal of Managed Care found that patients overwhelmingly prefer virtual visits to traditional office appointments when given the choice. Convenience, reduced travel time, shorter wait times, and quicker access to providers are major drivers. As health systems aim to enhance patient satisfaction and engagement, telehealth will continue to play a critical role in meeting these expectations.
- Convenience and Flexibility
For both patients and providers, telemedicine offers unmatched flexibility. Patients can consult a doctor without leaving home, saving on travel, childcare, or missed work. For physicians, virtual care can improve time management, allowing them to see more patients in a day and reduce administrative overhead. This efficiency translates into improved continuity of care, fewer no-shows, and more initiative-taking chronic disease management benefits that are too compelling to abandon.
- Accelerating Technological Innovation
Post-pandemic, the digital health sector has exploded with innovation. Advances in video conferencing, EMR integration, AI diagnostics, and remote monitoring devices are making virtual visits more effective. New tools are emerging that integrate clinical decision support, automated transcription, and real-time vitals tracking all designed to mimic the in-office experience remotely. As technology improves, the range of conditions that can be effectively managed through telehealth continues to grow.
- Reimbursement and Regulatory Support
Initially, reimbursement was a significant barrier to telehealth adoption, but this has changed. During the pandemic, Medicare expanded coverage for virtual visits, and many private insurers followed suit. While permanent parity laws are still evolving, the writing is on the wall: reimbursement models will continue to adapt to the demand for virtual care. Many U.S. states have passed telehealth parity laws, and CMS (Centers for Medicare & Medicaid Services) continues to explore ways to sustain expanded telehealth services.
- Promoting Health Equity
Telehealth holds immense promise for improving healthcare access in underserved areas. For rural populations, where clinics and hospitals may be hours away, virtual care brings critical services closer. It also helps urban residents with limited mobility, transportation issues, or restrictive work schedules. Smartphones have become a powerful tool for care delivery. Since most Americans including Black, Hispanic, and lower-income groups own smartphones, telehealth platforms that work on mobile devices are helping bridge the digital divide.
A Global Movement Toward Virtual Care
Telehealth is not just a U.S. phenomenon. According to the Future Health Index Report (2021):
- 64% of global healthcare leaders are investing heavily in virtual care.
- The U.S. (89%), Netherlands (83%), and Saudi Arabia (81%) lead in digital health investments.
Healthcare executives around the world view virtual care as a transformational force, particularly for specialties like stroke management, behavioral health, neurology, and cardiology.
Social Determinants of Health: Telehealth as a Bridge
Telehealth can help address social determinants of health factors that influence how individuals access and receive care. These include:
- Cultural hesitations toward seeking care
- Language barriers
- Geographic isolation
- Transportation challenges
- Work-related constraints
- Financial limitations
Virtual care, when implemented thoughtfully, helps lower these barriers by allowing patients to connect with providers without disrupting their daily lives. It also supports multilingual interfaces, flexible scheduling, and community-based care models.
The Numbers Tell the Story
The early months of the pandemic marked a watershed moment for virtual care:
- In 2020, over 1 billion virtual care visits took place, 500,000 for COVID-19 alone.
- Telehealth usage surged by 64.3%, representing a seismic shift in care delivery.
- The U.S. telehealth market, once valued at USD 3 billion, is now projected to reach USD 250 billion, according to reports.
These numbers suggest that while in-person visits will remain critical, hybrid care models combining in-person and virtual visits are becoming the norm.
Beyond COVID: What’s Next for Telehealth?
While COVID-19 forced healthcare systems to rapidly adopt telehealth, the coming years will be defined by intentional, strategic integration. Future directions include:
- Virtual-first primary care models, where patients begin all encounters online
- Integrated digital health ecosystems combining telehealth, RPM, and AI
- Value-based reimbursement tied to outcomes, not visit volumes
- Remote surgery preparation and post-op follow-up via virtual check-ins
- Cross-border telemedicine, enabling care across national boundaries
In addition, employers are increasingly offering telehealth benefits as part of corporate wellness programs, boosting access and reducing absenteeism.
Conclusion: Telehealth Is the New Healthcare Normal
Telehealth is not a temporary workaround; it is a foundational pillar of modern healthcare. The pandemic accelerated its adoption, but the long-term drivers are convenience, cost-effectiveness, patient demand, and technology ensuring that it will remain a vital part of the care continuum.
While challenges remain such as ensuring equitable broadband access, refining reimbursement policies, and safeguarding data privacy, telehealth’s trajectory is unmistakable. It is personal, scalable, and here to stay. Healthcare is unlikely to return to its pre-pandemic norms and that is a good thing. The transformation we are witnessing is not just necessary; it is a meaningful step toward a more accessible, efficient, and patient-centered system.





