HOME > BLOGS > CAN YOU SWIPE AWAY DEPRESSION? THE REAL STORY BEHIND THERAPY APPS
Can You Swipe Away Depression? The Real Story Behind Therapy Apps
Published Date: September 5, 2025
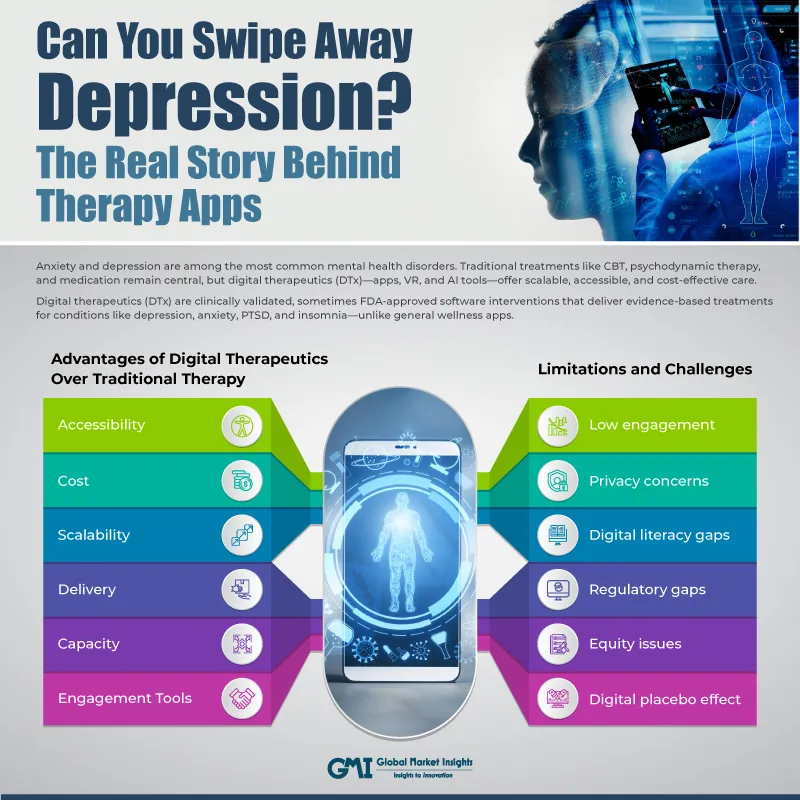
Mental health disorders, particularly anxiety and depression, are among the most prevalent and debilitating conditions globally. Traditional therapy primarily face-to-face cognitive behavioural therapy (CBT), psychodynamic therapy, and pharmacological interventions has long been the cornerstone of treatment. However, the digital revolution has introduced a new paradigm: Digital Therapeutics (DTx), including mobile apps, virtual reality (VR), and AI-powered platforms. These tools promise scalable, accessible, and cost-effective mental health care. But how do they compare to traditional therapy in terms of efficacy, engagement, and long-term outcomes?
Understanding Digital Therapeutics
Digital therapeutics are software-based interventions that deliver evidence-based treatments for medical and psychological conditions. Unlike general wellness apps, DTx are often clinically validated, sometimes FDA-approved, and designed to treat specific disorders like depression, anxiety, PTSD, and insomnia.
Key Modalities in DTx for Mental Health:
- Clinical validation: DTx products are supported by peer-reviewed research and RCTs.
- Regulatory oversight: Many meet standards set by bodies like the FDA, EMA, or MHRA.
- Targeted outcomes: Designed to treat specific conditions such as depression and anxiety, not just promote general well-being.
- Integration with care: Can be prescribed by healthcare professionals and reimbursed by insurance in some countries.
These tools can be standalone or used alongside traditional therapy, forming a blended care model.
Common Digital Therapeutic Modalities for Anxiety and Depression
App-Based CBT Programs
These apps deliver structured Cognitive Behavioral Therapy (CBT) modules through interactive lessons, videos, quizzes, and journaling exercises. They are designed to help users identify negative thought patterns, challenge cognitive distortions, and develop healthier coping strategies.
- Mimics the structure of traditional CBT sessions, often broken into weekly modules.
- Accessible anytime, self-paced, and often includes progress tracking.
- MoodGym—a pioneering CBT app developed by the Australian National University, offering exercises to manage depression and anxiety.
Many of these apps are backed by clinical trials and are used as adjuncts to therapy or as standalone interventions for mild to moderate symptoms.
AI-Powered Chatbots
AI chatbots simulate therapeutic conversations using natural language processing and machine learning. They provide real-time emotional support, mood tracking, and coping strategies based on CBT, dialectical behavior therapy (DBT), and mindfulness principles.
- Uses conversational AI to engage users in reflective dialogue, often with daily check-ins.
- Available 24/7, non-judgmental, and can reduce stigma associated with seeking help.
- Woebot—a clinically validated chatbot that delivers CBT-based support and has shown efficacy in reducing depressive symptoms in randomized trials.
These tools are especially useful for early intervention and emotional regulation between therapy sessions.
Mindfulness and Meditation Platforms
These platforms focus on reducing stress and anxiety through guided meditation, breathing exercises, body scans, and mindfulness practices. They often include programs tailored to specific issues like sleep, focus, or emotional regulation.
- Activates the parasympathetic nervous system, reducing cortisol levels and improving emotional resilience.
- Enhances self-awareness, reduces rumination, and improves sleep quality.
- Headspace—offers science-backed meditation programs and has partnered with healthcare providers to integrate mindfulness into clinical care.
Mindfulness-based digital interventions have been shown to significantly reduce symptoms of anxiety and depression, especially when practiced consistently.
Digital CBT for Insomnia (dCBT-I)
Insomnia is a common comorbidity with anxiety and depression. dCBT-I programs target sleep hygiene, cognitive restructuring around sleep beliefs, and behavioral strategies like stimulus control and sleep restriction.
- Addresses dysfunctional sleep patterns and beliefs that exacerbate mood disorders.
- Improves sleep quality, which in turn reduces depressive and anxiety symptoms.
- Sleepio—a digital CBT-I program with strong evidence from randomized controlled trials showing improvements in both sleep and mood.
Improved sleep has a cascading effect on emotional regulation, energy levels, and cognitive function.
Virtual Reality (VR) Exposure Therapy
VR therapy creates immersive environments that simulate anxiety-provoking scenarios, allowing patients to confront fears in a controlled, gradual manner. It is particularly effective for phobias, PTSD, and social anxiety.
- Facilitates exposure therapy by recreating real-world triggers in a safe digital space.
- Enhances engagement, allows for precise control of stimuli, and reduces avoidance behaviors.
- Oxford VR—offers VR-based exposure therapy for social anxiety and has demonstrated significant symptom reduction in clinical trials.
VR therapy is gaining traction in clinical settings due to its ability to personalize and intensify therapeutic experiences.
Biofeedback and Sensor-Integrated Tools
These tools use wearable devices to monitor physiological signals such as heart rate variability (HRV), skin conductance, and respiration. The data is used to provide real-time feedback and guide users through relaxation or breathing exercises.
- Helps users recognize stress responses and learn self-regulation techniques.
- Empowers users to manage anxiety proactively, improves emotional awareness.
- Muse—a brain-sensing headband that provides EEG-based feedback during meditation, helping users track and improve focus and calmness.
Biofeedback tools are especially useful for individuals with high physiological reactivity to stress and anxiety.
The Rise of Mental Health Apps
The digital therapeutics market has grown exponentially in the last decade. In 2023, the market value was USD 8.9 billion, with a projected CAGR of 31.5%. This surge reflects a global shift toward technology-enabled care, especially in response to rising mental health challenges and limited access to traditional therapy.
Today, there are over 50,000 mental health apps available across app stores, offering everything from mood tracking and meditation to AI-powered therapy simulations. However, only about 2% of these apps have published clinical evidence supporting their effectiveness, raising serious concerns about quality control, safety, and therapeutic validity. The lack of regulation and standardized evaluation frameworks means users often face difficulty distinguishing between evidence-based tools and unverified wellness products. This underscores the urgent need for clinical vetting, regulatory oversight, and integration of digital therapeutics into formal healthcare systems to ensure that innovation translates into safe, effective, and equitable mental health support.
Adoption and Engagement Trends
While initial interest in mental health apps is high, sustaining user engagement remains a significant challenge. Studies show that 74% of users stop using health apps after just ten uses, and apps like PTSD Coach experience a dramatic drop-off, with only 14% of users remaining active after the first day. This steep decline highlights a critical gap between accessibility and sustained therapeutic impact. Common reasons for disengagement include poor usability, such as confusing interfaces or technical glitches, lack of personalization that fails to adapt to individual needs, privacy concerns over sensitive mental health data, and low perceived effectiveness when users do not experience meaningful improvements. These issues suggest that while digital therapeutics (DTx) offer unprecedented reach, their long-term success depends on thoughtful design, clinical integration, and continuous user support. For developers and clinicians alike, the challenge is not just to create accessible tools, but to build engaging, trustworthy, and clinically effective experiences that users will return to consistently.
Clinical Effectiveness: Apps vs. Traditional Therapy
While initial interest in mental health apps is high, engagement drops sharply over time. In 2021, a meta-analysis of thirty-nine randomized controlled trials (RCTs) involving 9,751 adults revealed:
- Internet-based CBT (iCBT) was effective in reducing depressive symptoms.
- Guided iCBT (with therapist support) showed stronger effects for moderate-to-severe depression.
- Unguided iCBT still provided significant and lasting benefits for mild-to-moderate symptoms.
Another meta-analysis of 54 RCTs involving 5,463 patients compared therapist-guided remote CBT with in-person CBT:
- Found no significant difference in effectiveness for treating anxiety, depression, insomnia, or chronic pain.
- Supports the viability of remote CBT as a clinically equivalent alternative to traditional therapy.
Case Study:
- Headspace vs. SilverCloud
A 2022 RCT with 2,079 participants, tested five digital interventions:
Apps: Headspace, SilverCloud, and versions with Enhanced Personalized Feedback (EPF).
Results after 6 weeks:
- PHQ-9 scores dropped by 2.1–2.9 points (depression)
- GAD-7 scores dropped by 1.5–2.1 points (anxiety)
- No single app was superior, suggesting multiple digital approaches can be effective.
- The Special Case of Digital CBT for Insomnia
Sleep and mood disorders are deeply interconnected. Studies show that dCBT-I not only improves sleep but also:
- Reduces insomnia symptoms two times more effectively than online sleep education.
- Reduces depressive symptoms 2.5x more than controls.
Advantages of Digital Therapeutics Over Traditional Therapy
- Accessibility: Digital therapeutics are available 24/7 and can be accessed globally, offering support beyond traditional office hours and geographical constraints. This is especially beneficial for individuals in remote areas or with irregular schedules.
- Cost: Many mental health apps are free or come at a lower cost than traditional therapy, and some are reimbursed by insurance. In contrast, in-person therapy can be expensive and often requires out-of-pocket payments.
- Scalability: Digital tools can be deployed to millions simultaneously without requiring additional therapists, making them ideal for large populations and public health initiatives.
- Delivery: These tools use algorithm-driven personalization to adapt content based on user behavior and preferences, whereas traditional therapy relies on clinician expertise and manual customization.
- Capacity: Unlike traditional therapy, which is limited by therapist availability and session slots, digital therapeutics can support unlimited users concurrently, reducing wait times and improving access.
- Engagement Tools: Apps often include gamification, reminders, progress tracking, and interactive exercises to keep users engaged, while traditional therapy typically relies on verbal interaction and homework assignments.
Limitations and Challenges
- Low engagement: Despite initial interest, most users discontinue use quickly without sustained motivation or external support. This limits long-term therapeutic impact.
- Privacy concerns: Some apps lack robust data encryption or clear privacy policies, raising concerns about the handling of sensitive mental health information.
- Digital literacy gaps: Not all users are comfortable navigating digital platforms, especially older adults or those with limited tech exposure, which can hinder adoption and effectiveness.
- Regulatory gaps: Many mental health apps are not clinically validated or approved by regulatory bodies, making it difficult to assess their safety and efficacy.
- Equity issues: Individuals in rural or low-income communities may lack access to smartphones, stable internet, or digital infrastructure, creating disparities in who can benefit from these tools.
- Digital placebo effect: Some perceived benefits may stem from novelty or user expectations rather than actual therapeutic content, complicating the evaluation of true clinical outcomes.
Blended Care: The Future of Therapy
Blended care combines digital tools with human-led therapy to:
- Provide continuous support between sessions.
- Personalized interventions based on real-time data.
- Scale mental health services without losing human touch.
Role of AI in Blended Care:
- Predict relapse risk using behavioral data.
- Deliver “just-in-time” interventions when symptoms spike.
- Adapt therapy content dynamically for each user.
User Experience Matters:
- A review of 13,549 user reviews across 106 mental health apps revealed:
- Top reason for abandonment: Poor usability and lack of personalization.
- Apps with adaptive content and diverse resources had higher ratings.
- Privacy and trust remain non-negotiable for long-term use.
Regulation and Reimbursement: A Turning Point
In 2025, the Centers for Medicare & Medicaid Services (CMS) introduced new reimbursement codes for Digital Mental Health Treatment (DMHT):
- HCPCS G0552: Supply and onboarding of DMHT devices: This code allows healthcare providers to bill for the initial setup and supply of digital mental health treatment (DMHT) devices. It covers onboarding activities such as patient education, device configuration, and integration into care plans. This step ensures that patients are properly equipped and informed to use digital therapeutics effectively.
- G0553 and G0554: Monthly billing for treatment management: These codes support ongoing reimbursement for monthly monitoring and management of patients using DMHT tools. They include reviewing patient data, adjusting treatment protocols, and providing remote support. This enables clinicians to maintain continuity of care and track progress without requiring in-person visits.
To qualify for reimbursement, DMHT devices must be either FDA-cleared under existing regulatory pathways or granted De Novo authorization for novel technologies. This requirement ensures that only clinically validated and safe digital therapeutics are integrated into reimbursable healthcare services, marking a significant move toward mainstream adoption and quality assurance.
Clinical Implications
For Clinicians:
- Use DTx for mild to moderate cases as standalone or adjuncts.
- Monitor app engagement and adjust recommendations.
- Educate patients on choosing reputable apps with strong privacy policies.
For Researchers:
- Conduct long-term, large-scale studies.
- Identify mechanisms of change such as CBT more effective than mindfulness for certain subgroups.
- Investigate the digital placebo effect.
For Policymakers:
- Establish stricter validation frameworks.
- Ensure equitable access across demographics.
- Support insurance reimbursement for validated tools.
Conclusion: Digital therapeutics are reshaping mental health care
Mental health care is no longer confined to the therapist’s office—it is evolving into a dynamic, tech-enabled ecosystem. As anxiety and depression continue to affect millions globally, the emergence of digital therapeutics marks a pivotal shift in how care is delivered, accessed, and experienced. This transformation is not just about convenience; it is about redefining the future of mental health treatment.
For healthcare systems, ignoring the potential of digital therapeutics means missing out on scalable solutions that can reduce wait times, lower costs, and improve outcomes. Studies show that app-based interventions and remote CBT can match the effectiveness of traditional therapy for mild to moderate cases, while offering unmatched accessibility and personalization. The cost of inaction—continued stigma, untreated symptoms, and overwhelmed clinical resources—is simply too high.
For mental health professionals, this shift demands a new mindset: one that embraces blended care models, leverages AI for personalization, and integrates digital tools into routine practice. For patients, it signals a future where support is available anytime, anywhere, empowering individuals to take control of their mental health journey.
The move from reactive crisis management to initiative-taking, tech-driven support is one of the most significant opportunities to improve both individual wellbeing and system-wide efficiency. The question now is: Are we ready to invest in the digital mental health revolution that could transform lives and save billions?
The future of mental health care depends not only on clinical expertise but on our ability to innovate, adapt, and scale. Digital therapeutics are not a replacement—they are a powerful complement. And the time to act is now.
Author: Mariam Faizullabhoy